Category: Nurse’s Corner
Nurse Encourages Mesothelioma Families to Advocate for Their Loved Ones
I have taken care of mesothelioma patients for many years. To be honest, some patient’s stories stay with me more than others. I recently cared for this woman who had a high school degree and had a pretty simple life. I mean she was not consumed like the average American about having material things and constantly wanting more. We will call her Sally. Sally accepted life on life’s terms.
Unfortunately, she was diagnosed with mesothelioma with a routine chest X-ray. She was not symptomatic and was able to work, but she had become one of the many victims of this dreaded disease. As I cared for her she had been in the hospital for one month after being discharged for a few days to rehab. Her surgery had not gone along as planned, and basically her cancer was unresectable, or in other words, her cancer was inoperable. Sally was short of breath and it was difficult for her to do much. She also had a very poor appetite.
Her family loved her very much, but like her, they all just accepted her symptoms as normal. I felt like there was no one person who was advocating for her. We all know how important nutrition is. Her wound was poorly healed, secondary to lack of nutrition and her disease progress. I felt like I needed to speak for Sally and to help her overcome some of these issues. I don’t think she knew the importance of nutrition, and I felt that giving her some basic information could make a difference.
Although she refused a meal tray, I offered her a frappe and encouraged her to drink it. I even held the cup to her lips so it would be easy for her to drink. Sure enough within a few hours she had drank the high calorie frappe. I consulted a nutritionist to get her input as well. I believed that Sally’s wound could heal, but she would need some dressing changes and careful observation. We called the thoracic surgeon so he could give his input. I guess when I think of Sally, I feel like someone has to watch and advocate for her and for all mesothelioma patients.
The definition of advocate is to speak, plead or argue in favor of someone. There are people who are available to be advocates. Advocates can sometimes be a significant other, family or friend. The nurse can be the advocate while a person is in the hospital, but once they leave they need someone to travel the road with them. It is difficult to think of everything someone needs during a battle with mesothelioma, but having someone fighting with the patient and for the patient can help keep the patient’s recovery progressing.
If you don’t have a family member who can advocate for you, consider asking your primary care physician, friend, legal team or your mesothelioma medical team for support or suggestions.
If you have questions about your mesothelioma treatment or any aspect of your mesothelioma care, please contact us.

Communicating with Mesothelioma Medical Team Can Help Ease Discomfort
“I am a little short of breath, but I didn’t call anyone because I was thinking it would get better.” “I am still having pain, but I thought it would go away.” Two very different patients; two very common problems for patients with mesothelioma.
This past weekend I saw two patients who had both undergone surgery a month ago, and both had very different symptoms that could be helped. Except they did not bring these issues to the medical team’s attention, instead they suffered in silence at home until their next scheduled appointment. While I know it is scary to leave the hospital where you are surrounded by professionals who know what is typical and what is not, it is important that mesothelioma patients be aware of subtle, bothersome changes that can be treated before they develop into bigger problems.
Recovering from surgery is a very stressful time. Dealing with pain, dietary restrictions and exercise guidelines are tough enough, but add to them management of suture lines, fluid balance, weakness, and even bowel function, and patients can easily become overwhelmed. Although a patient may not know what is “not normal” after surgery, any time you are concerned about something, it is best to call your medical point of contact to help allay your fears, and maybe even get relief through a medication or additional information.
The first patient had developed shortness of breath over a couple of days. In her case, she was not discharged with a diuretic- intentionally. But after a call to her doctor and a short discussion, a prescription was ordered and she was “much better” the next day.
For the patient suffering from pain, ongoing discussions between him and the medical team has allowed the doctor to monitor dosage and adjust medication as needed. Adding an additional medication, taking the medication as needed, and developing a plan all helped to ease the pain and allow the patient to rest easier.
Every patient’s journey with mesothelioma is different, but all of them will experience bumps along the way. Open communication with your medical team, your family, and your caregivers is essential. Your team will be responsive to your needs – but they need to know about them. If something is bothering you, ask. Your team wants you to feel the best you possibly can!
If you have questions about your mesothelioma treatment or any aspect of your mesothelioma care, please contact us.
Know more about Mesothelioma and how you can deal with it.
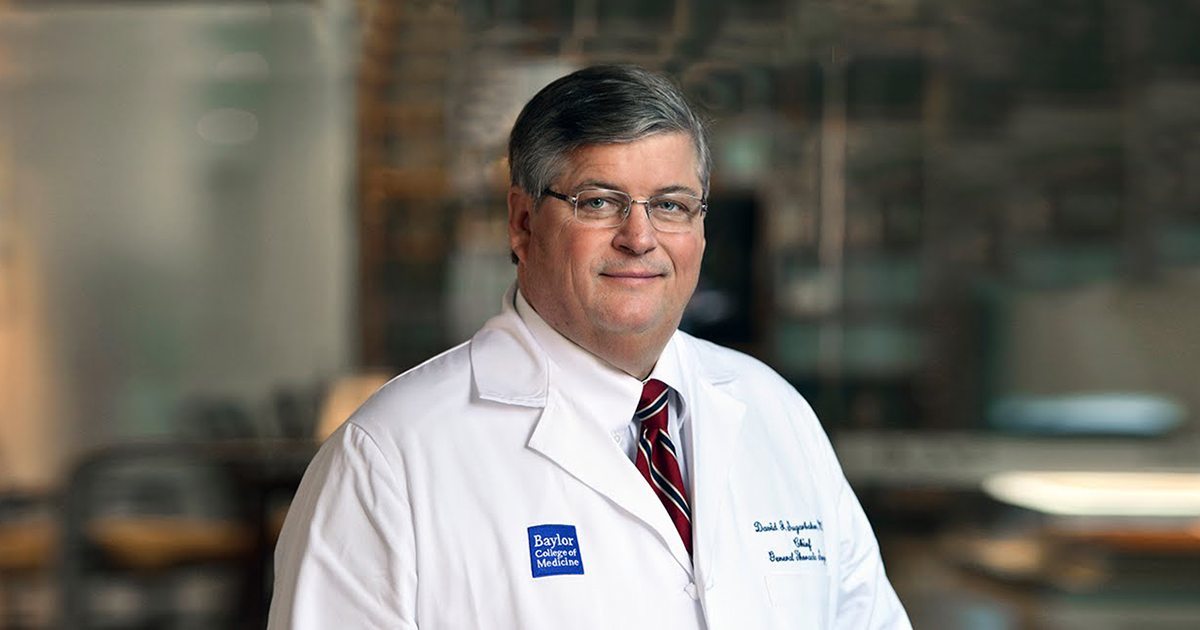
Dr. Sugarbaker’s Legacy at Boston’s Brigham & Women’s Hospital
News is quickly spreading that Dr. David Sugarbaker will step down from his position as the Chief of Thoracic Surgery at Boston’s Brigham & Women’s Hospital effective April 30. Dr Sugarbaker is best known for his relentless fight against mesothelioma.
As a staff nurse who had the pleasure of working alongside Dr. Sugarbaker for the past 20 years, I feel honored and privileged to have had that opportunity. I could certainly go on and on about what a wonderful physician he is and how much he cares, but the bottom line is that he will be sorely missed. Dr. Sugarbaker was truly passionate about his patients he cared for and he did everything within his power to help them win the war against mesothelioma.
During his daily rounds to the ICU and other floors, his energy and radiance set the tone for the day, and that enthusiasm will be hard to replace. His presence was almost electrifying. He would offer hope to the sickest of the sick convincing the patients to move forward. The patient response was remarkable.
Dr. David Sugarbaker has accepted a new position as Director of the Texas Lung Institute at the Baylor College of Medicine and Chief of Thoracic Surgery in the Michael E. DeBakey Department of Surgery. He also will be named as The Olga Keith Wiess Professor of Surgery, Baylor College of Medicine.
Selfishly, all of us at Brigham and Women’s Hospital will miss him, but I believe the mesothelioma world will benefit greatly by sharing his expertise outside of Boston. Perhaps this played into Dr. Sugarbaker’s decision to move on, and I respect that decision.
During his 25 years of service at Brigham and Women’s, Dr. Sugarbaker has made significant contributions to patient care, research and teaching which include the establishment of the first lung transplant program in New England. He also founded the International Mesothelioma Program at Brigham.
Dr. Sugarbaker first came to Brigham in 1979 as a surgical resident. Upon completion of his residency in 1986, he left to obtain cardiothoracic training at the University of Toronto. He returned to Brigham and Women’s in 1988 as the Chief of the newly formed Division of Thoracic Surgery, a program which is now recognized as one of the best in the nation.
Dr. Sugarbaker has been focusing on pleural mesothelioma since 1988, and his contributions to the treatment of this devastating disease have helped countless patients and families who had no other options. In 2002, he founded the International Mesothelioma Program with the primary goal of finding a cure for this disease. This program is the largest of its kind and attracts patients from around the world.
Dr. Sugarbaker played a leading role in the establishment of the Tissue and Blood Repository at Brigham and Women’s Hospital in 1989. This was one of the first tissue repositories in the U.S. and has led to extremely fruitful collaborative research projects. He is deeply committed to teaching the next generation of physicians and has mentored hundreds of residents and fellows during his time at Brigham and Women’s. His contributions to education also include the establishment of a unique fellowship in thoracic oncology and a minimally invasive thoracic surgery fellowship, as well as a visiting scholar program for Thoracic Surgery.
Sources:
- Thoracic Surgery in the Michael E. DeBakey Department of Surgery
https://www.bcm.edu/departments/surgery/divisions/cardiothoracic-surgery - founded the International Mesothelioma Program with the primary goal of finding a cure for this disease
http://www.brighamandwomens.org/Departments_and_Services/surgery/thoracic-surgery/mesothelioma/default.aspx - The Olga Keith Wiess Professor of Surgery, Baylor College of Medicine
https://www.bcm.edu
Mesothelioma Patient Turns the Corner on Her Recovery
 Last week the mesothelioma patient we have been following for several weeks was still very sick with infections, air leaks, and respiratory failure she developed after her surgery. She was very depressed, as was her family, as they were not expecting such a rough recovery. The family has been very frustrated, and they started second-guessing their decisions and began to wonder what their loved one really wants for her care. They held a family meeting where they decided to re-assess in one more week. Fortunately, there have been small but steady gains during the last week – the woman’s infections have subsided, she is gaining strength and her attitude has become more positive.
Last week the mesothelioma patient we have been following for several weeks was still very sick with infections, air leaks, and respiratory failure she developed after her surgery. She was very depressed, as was her family, as they were not expecting such a rough recovery. The family has been very frustrated, and they started second-guessing their decisions and began to wonder what their loved one really wants for her care. They held a family meeting where they decided to re-assess in one more week. Fortunately, there have been small but steady gains during the last week – the woman’s infections have subsided, she is gaining strength and her attitude has become more positive.
In talking with her husband and daughters, who are in their early twenties, I got to know what kind of person the woman is as well as how much this sickness is affecting them too. Finding themselves in the role of caregivers is foreign territory. When asked to describe what their day looks like, they explained that it starts early with a call to the ICU to see what kind of a night their loved one had. Then it is on to the hospital where they spend as much time as possible with their wife and mother. It includes time spent in the waiting room with family members of other patients, some much older patients with mesothelioma who are doing better than their loved one. Then they meet with the doctors for their daily update.
Thankfully, their loved one has a team of primary nurses who know her well and feel like part of the family at this point. Today, one of their favorite nurses is on duty. She is upbeat and personable – does she have any idea what that means to them? They say they do not have to worry about the “numbers” or their mother being too sick to ambulate – when they know this is vital to any chance at recovery. The hours go by slowly. They talk about how they try to deal with so much uncertainty – their wife/mother is the ‘director’ of the family and she guides them all through life. She would be the one who could tell them if they should go back to work or school, or if they should spend so much time with her. They want her to help direct them as to what to do now.
There have been guidelines all along for patients without complications; but their case is unique. Uncertainty clouds every decision. What if one goes back to school and their mother takes a turn for the worse and dies? Should they be thinking like that- it is reality- that it is a possibility. They describe being paralyzed with indecision as they wait for their “director” to tell them what to do. Mostly, they describe a situation so foreign to anything they have gone through as individuals or a family.
Emotional exhaustion has turned to physical exhaustion for all of them. They play the ‘what if’ game. What if she recovers, but she is in pain? What if her infections get worse, should they continue the same treatment? All those conversations about what she would and would not want are echoing in their heads. Luckily, their loved one’s health is improving.
Mesothelioma has been held at bay for another day.
If you have questions about your mesothelioma treatment or any aspect of your mesothelioma care, please contact us.
Family of Mesothelioma Patient Faces Tough Decisions
This week we continue to follow a woman who is recovering from surgery after being diagnosed with mesothelioma. She has been struggling more than expected, and the family is trying to come to terms with the extended care needed to get their loved one back on her feet. The patient is critically ill and has many medical issues that need to be managed, and her family members are feeling lost.
They remember being told something about their loved one facing potential complications from surgery, but nothing could have prepared them for all this. Serious infections, respiratory issues, and most upsetting to them, the patient is very depressed and has lost all hope. Everything is a major effort- from acknowledging her family to asking for water- and it is painful for them to watch.
When things do not go as we expect and medical decisions need to be made, the most important thing a family member can do is to listen and to keep in mind what the patient told you in the past. What are their wishes? Those difficult “what if” and “I never want xxx care” conversations are all running through your mind. It is vital at this point in your loved one’s illness, that you remember their wishes and keep the lines of communication open with your healthcare team.
Now, it is excruciating to watch their family member struggle to talk and to perform the most basic human functions and they can’t believe that she will ever get better. The truth is while some patients do recover, some may not. Recovery goals are set each day in the ICU, and measuring the patient’s progress against them is one way to assess how the patient is progressing.
In our patient’s case, after two family meetings involving the health care team, some decisions are made. After much discussion and listening and praying the family has decided to keep going with treatment and to re-evaluate in one week. Now, the family is praying for improvements in their loved one.
Although to let you realize how grave the situation is, the decision has been made not to perform CPR if her heart stops. From the medical standpoint the treatment and care is aggressive, and the medical team likes to know they have exhausted all options. From the family’s perspective, they would like to see their loved one comfortable and at rest.
Next week we will offer an update as we continue to follow this patient.
If you have questions about your mesothelioma treatment or any aspect of your mesothelioma care, please contact us.
Know more about Mesothelioma and how you can deal with it.
Free Mesothelioma Patient & Treatment Guide
We’d like to offer you our in-depth guide, “A Patient’s Guide to Mesothelioma,” absolutely free of charge.
It contains a wealth of information and resources to help you better understand the condition, choose (and afford) appropriate treatment, and exercise your legal right to compensation.
Download Now