Mesothelioma Hospice and Pallative Care

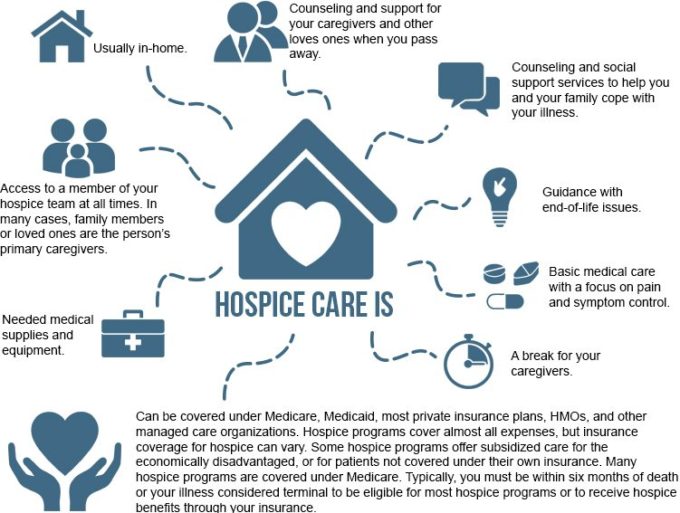
Hospice care is a type of medical service that includes emotional support and spiritual resources for the terminally ill and family members of the Terminally Ill.
It focuses on caring, not curing. It helps family members manage practical details and emotional challenges of caring for a dying loved one.
It gives patients the ability to choose what’s important to them. Hospice programs are offered in home or the uncommonly used hospice centers, such as a nursing home, hospital or long-term care facility.
Hospice programs keep the patient comfortable and improve the quality of life as much as possible. Hospice care is usually referred through a primary care physician and the patient is overseen by a team of hospice professionals.
It often relies on the family caregiver in addition to a visiting hospice nurse. Since hospice is usually provided in the home, Medicare hospice benefit provides necessary equipment and personnel. Medicare benefits will assume payment for medications related to the underlying disease.
Palliative Care
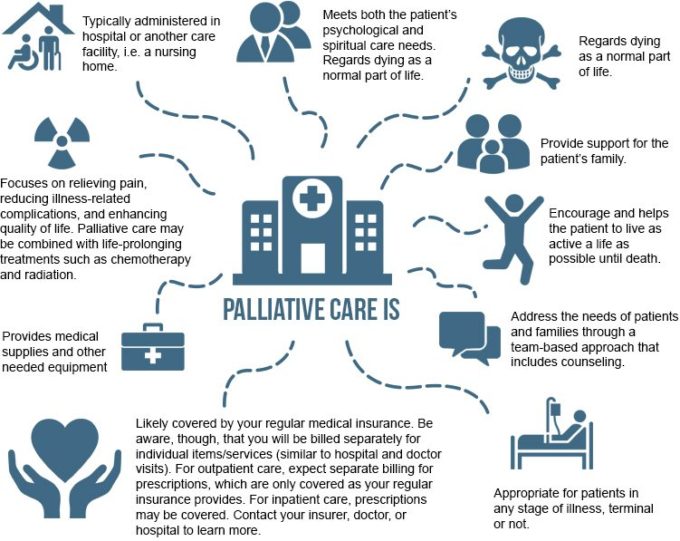
The World Health Organization defines palliative care as a healthcare approach focusing on improving the quality of life of patients and their families facing life-threatening illnesses.
It focuses on the prevention and relief of suffering by means of early identification assessment and treatment of pain, psychosocial and spiritual issues.
It requires training in subjects such as social issues and psychology. Palliative care nurses have a thorough knowledge of medications used for pain, symptom control, and psychiatric conditions.
The nurses work with the patient and share information to the treating physician. According to the Center to Advance Palliative Care, 53 percent of hospitals with 50 or more beds have a palliative care program.
The majority of palliative care in this country is provided on inpatient consultation service. Oncologynurseadvisor.com cites New York’s Mount Sinai Hospital team as an example.
The team has 1,200 consultations a year and is often called in by oncologists to see patients with such symptoms as nausea and vomiting, whether from cancer or its treatment.
The palliative care team helps patients complete advance directives like helping the patient choose a proxy decision-maker in the event they become unable to communicate their wishes about their medical care.
The team helps the patient speak to the proxy and the family about quality of life and about where and how the patient would like to be helped to optimize quality of life. Note: Because hospice and palliative care program guidelines differ, talk with your doctor about the best service for you.
More Hospitals Offer Mesothelioma Patients Palliative Care Options
Palliative care has been gaining momentum in the medical community as a critical step for many terminally ill patients.
For mesothelioma patients in the advanced stage of their cancer, turning to palliative care, which focuses on relieving symptoms and keeping the patient comfortable, offers them an opportunity to spend more time with their loved ones during their end of life.
Mesothelioma is one of the most aggressive and deadliest forms of cancer, with limited treatment options.
Symptoms may not appear until up to 50 years after initial exposure to asbestos, the only known cause of the disease. However, once symptoms become apparent, mesothelioma may rapidly progress to cause life-threatening complications.
The prognosis for mesothelioma patients is grim with the average survival time varying from 4 – 18 months after diagnosis.
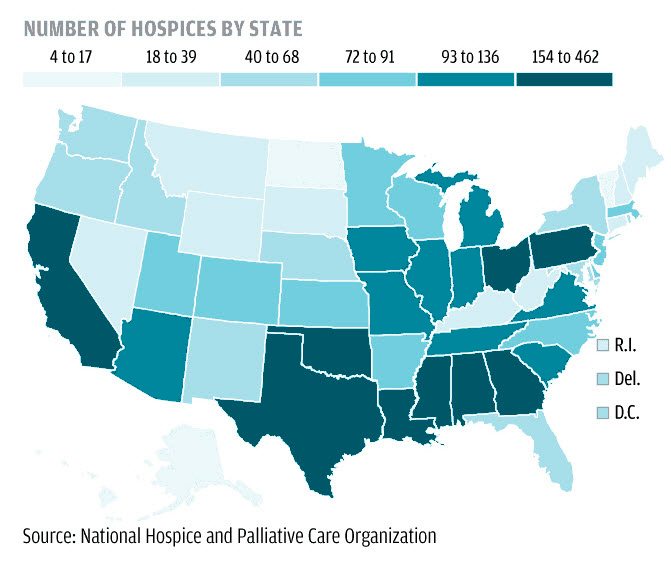
Now, according to a new study from the Center to Advance Palliative Care (CAPC), mesothelioma patients may have more palliative care options available to them. CAPC reports the number of U.S. hospitals with palliative care teams increased for the 10th consecutive year.
In 2010, there were 1,635 palliative care teams in hospitals in the United States, for an increase of 4.3% over 2009. CAPC reports palliative care has been one of the fastest growing trends in health care over the last ten years, growing nearly 150% since 2000.
66% of American hospitals now have palliative care teams. Hospitals in the northeast region of the U.S. have the highest percentage at 75.8%. The southern region of the U.S. offers the fewest palliative care options with just 52.7% of the hospitals reporting palliative care teams.
CAPC attributes the growth of palliative care “to the increasing number of Americans living with serious and chronic illnesses and to the caregiving realities faced by their families.”
In a separate study, Massachusetts General Hospital researchers attributed palliative care to increased survival rate among advanced lung cancer patients. The researchers cited improved mood and quality of life, as well as appropriate end-of-life care, for the improved survival rates.
MGH employs palliative care teams consisting of physicians, nurses, social workers and chaplains trained to help patients and their families facing terminal illness cope with the psychological and spiritual aspects of their disease, as well as managing symptoms.
Mesothelioma Caregivers
Patients diagnosed with malignant mesothelioma face a long, demanding battle involving countless doctors’ appointments, extensive tests, chemotherapy treatments and radiation therapy.
Managing the illness and all the appointments, on top of taking care of day-to-day living needs, is virtually impossible without the help of a dedicated caregiver.
Caregivers, typically spouses or other family members, usually provide constant care for mesothelioma patients during their treatments.
Caregiver duties can include:
- grocery shopping
- housekeeping
- preparing meals
- transportation
- meal preparation
- management of insurance forms
- medical forms and prescriptions
- general care for the patient as well as emotional support
For many caregivers this is all done while trying to care for other family members. Caregivers play such a vital role in medical care that each year November is named National Family Caregivers Month.
President Obama continued the tradition started in 1997 when President Clinton signed the first presidential proclamation recognizing the selflessness of caregivers.
According to the National Family Caregivers Association, more than 65 million family caregivers in this country fulfill a vital role on the care team. Some patients may feel like they are imposing on their loved ones for the extra care required as they recover from this type of cancer.
However, it is important that patients lean on their caregivers and keep a positive mental attitude. The love and support of those you trust can truly make a difference in your recovery.
Supporting a loved one going through cancer treatment is difficult. No one wants to see a friend or family member go through the challenges that come with cancer care, but to get to the other side and to get on with your lives, you and your loved one have to get through the hardship.
Talk to your loved one; let them know that you are there for them and that you are happy to be helping. Let them know it is not a burden for you and that your main priority is getting them well.
Being a caregiver can be stressful at times, but remember what an honor it is to help someone you love who is battling mesothelioma. You might also like to read

CanCare is a network of trained volunteers including cancer survivors, family members of cancer survivors and medical professionals who provide emotional support to others facing cancer.

Things I Wish I’d Known: No first-time caregiver should face cancer caregiving without this book in hand. It offers keys to unlocking the dilemmas of cancer caregiving so you can take charge as a knowledgeable advocate for your patient.

Cancer support using hypnotherapy
Things to Consider When Supporting your Loved One

Recognize that your friend and his family’s “behavior” may change. They will be feeling a wide range of emotions so understanding that and continuing to listen and talk to them through this difficult time is essential to their coping.

Focus on keeping your relationship balanced. While it is important to acknowledge your friend’s disease, not every conversation need be centered on their mesothelioma treatment. More than likely they want to talk about other things and find out how your life is going.

Ask the person with cancer directly what you can do to help. Don’t assume and don’t talk through their caregiver – they may have a special request for you.

Don’t forget about them. As their disease progresses and treatments continue friends may disappear just when the person needs them the most. Reach out and let them know you are thinking of them and are available to help if needed.
Questions to Ask Your Doctor to Maximize Health Care
Ueno also suggests being organized by having your questions well thought out and written down.
Following are some questions and comments he offers as a way to validate that you heard clearly what the doctor said and to help keep the conversation focused:
| “I don’t understand what you’re saying.” | If you don’t understand something the doctor said, simply say so. You may not have another opportunity to get the doctor’s undivided attention, so make sure you get clarity. |
| “Can you please explain that using simpler words?” | The doctor should be using words and terms you understand, or should clearly define them for you. |
| “My understanding is X; do I understand this correctly?” | Parrot back to the doctor what you think he said to make sure your understanding is correct. |
| “Did we agree to X, then Y, then Z?” | Make sure you understand the plan of action – and that you are comfortable with it. Being empowered means you get a say in your treatment plan. |
| What type and stage of mesothelioma do I have? | |
| How many mesothelioma cases have you treated? | |
| How many surgical procedures have you performed on mesothelioma patients? | |
| Do you believe I can be successfully treated? What does the treatment plan look like to you? | |
| How often will I receive treatments and how long will my course of treatment last? | |
| What are the possible benefits, risks, and complications associated with the mesothelioma treatments? | |
| How will I know if the treatment is effective? When will follow-up tests be done to check on the progress of my treatment? | |
| What is your philosophy and approach when my treatment options are unsuccessful or my condition worsens during treatment? | |
| Will you help me find a clinical trial? | |
| Can you recommend resources for additional information about mesothelioma? | |
| Do you mind if I get a second opinion? |
Sources:
- World Health Organization
http://www.who.int/cancer/palliative/definition/en - Naoto Ueno, M.D., Ph.D
https://www.mdanderson.org/publications/cancerwise/2012/03/ask-the-right-questions-get-the-most-out-of-your-oncology-appoin.html - Cancer support using hypnotherapy
https://www.bbbenefits.com.au/health-issues-list/cancer-support - CanCare
http://www.cancare.org - National Family Caregivers Association
http://www.caregiveraction.org - National Family Caregivers Month
http://www.huffingtonpost.com/news/national-family-caregivers-month - Center to Advance Palliative Care
https://media.capc.org/filer_public/e1/c9/e1c93c86-7fad-4aa6-b5e0-7757ef313da0/capc-growth-analysis-snapshot-2011.pdf - New York’s Mount Sinai Hospital team
https://www.mountsinai.org - Center to Advance Palliative Care
https://www.capc.org